Age-dependent manifestations and case definitions of pediatric Zika - a prospective cohort study
My take on the article
TL;DR: This article substantially advances the scientific understanding of Zika. Here, we show that the clinical profile of Zika changes across pediatric age, displaying a higher number and greater variety of sympmtoms in older children as compared to younger children. This phenomenon of increasing severity with age is likely to extend into adulthood. A large percentage of Zika cases manifest as afebrile rash. As current case definitions do not capture the full spectrum of Zika’s symptoms, many true Zika cases are missed by surveillance systems are are misdiagnosed.
Motivation: Zika in children remains an understudied aspect of the 2015-2015 Zika pandemic. This study therefore aimed to answer two central questions: 1) What is the clinical spectrum of Zika in children? and 2) How accurate are Zika case definitions that were put forward by the World Health Organization (WHO) and the Pan American Health Organization (PAHO) in children?
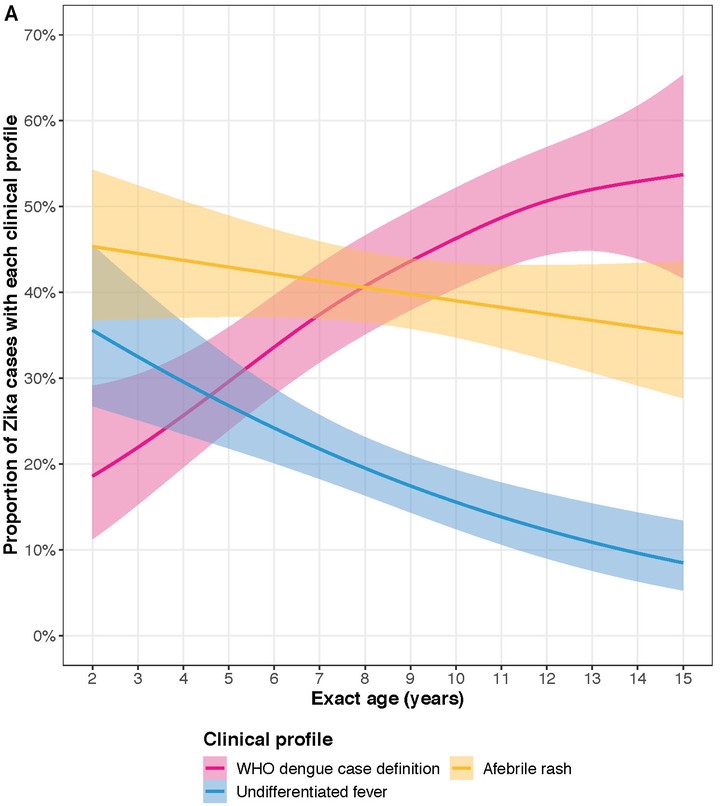
Methods: To answer these questions, we prospectively followed ~3,700 children (aged 2 - 14) in the Pediatric Dengue Cohort Study in Managua, Nicaragua during the city’s Zika epidemic (January 2016 - February 2017). We confirmed 556 Zika cases by PCR and a serological algorithm. We categorized the Zika cases into 3 broad groups, depending on their clinical profile: 1) Zika cases meeting the WHO dengue case definitions, 2) Zika cases manifesting with undifferentiated fever, and 3) Zika cases present with afebrile rash. We then analyzed the Zika cases’ symptoms.
Results: Only 20%-30% of the Zika cases were captured under the WHO and PAHO case definitions. A full 60% of the Zika cases did not meet any of the WHO case definitions for dengue, even though Zika is supposed to resemble dengue. Interestingly, 40% of Zika cases presented with afebrile rash, a clinical profile that is supposedly atypical. These findings were explained by the increasing prevalence of a Zika signs and symptoms across pediatric age. Zika in younger children tended to presented as afebrile rash or undifferentiated fever, whereas Zika in older children presented as afebrile rash or resembled a traditional case of dengue. Rash, fever, arthralgia, leukopenia, cervical lymphadenopathy, and other clinical features displayed increasing (and sometimes non-linear) increases in prevalence with age. Consequently, the WHO and PAHO case definitions had a higher sensitivity in older children as compared to younger children. We showed our results held independent of prior dengue virus infection, suggestion that a mild form of antibody-dependent enhancement does not explain our results.
Interpretation: Our work is the largest and most thorough assessment of Zika in children. Current case definitions for Zika, and hence the clinical understanding of the disease, are too narrow. Many true Zika cases have likely been missed by surveillance systems and misdiagnosed, implying the existence of large, systematic biases throughout the epidemiological literature of Zika. Children (and young children, in particular) are likely to have been the most missed group; because these children would still be infectious, children with Zika represent a hidden reservoir of infection that has not been previously recognized. Our results present major challenges to existing standards for the diagnosis, surveillance, and control efforts of Zika. An urgent need therefore exists to revisit case definitions for the disease and update our collective scientific understanding of Zika.
Article availability: The freely available article can be found here and a tweetorial on this article is available over here. If you have trouble accessing the article or wish to ask a question about it, please contact me.